Unpacking the Geography of America’s Youth Suicide Epidemic
The dangers and challenges young people in the United States face are well-known. Gangs and online predators are the subject of podcasts and newsmagazines. And the continuing list of school shootings, from Columbine to Parkland, has sadly become familiar to Americans.
But for many young people, the bigger danger comes from within, in the form of self-harm. Other than unintentional injury, suicide is the leading cause of death for Americans ages 10 to 24, according to the Centers for Disease Control. In 2019, the number for suicide was higher than for homicide, influenza, and liver disease combined in that age group, according to the CDC.
And the problem has only gotten worse for young people in the United States. In the period from 2000–2004, there were 7.0 suicides per 100,000 people in the 10- to 24-year-old age group. By 2015–2019, the figure had climbed to 10.03. That’s an increase of 43%, nationally.
To understand the scale of the challenge, the American Communities Project worked with Center on Rural Innovation to analyze 20 years of suicide figures from the CDC’s WONDER database. That analysis found that suicide rates among young people had risen in every one of the ACP’s 15 community types over that time, from the densely-packed Big Cities to the sparsely-populated Aging Farmlands and everything in between. The work, funded by a grant from the Arthur Blank Family Foundation to study Deaths of Despair in America, shows just how deep the nation’s suicide epidemic goes.
Looking through the ACP’s prism of 15 community types, clear place-based patterns emerge for the suicide rates among 10- to 24-year-olds, the focus of this report.
- Rural communities have seen some of the highest rates in suicide in the age group and some of the biggest increases since 2000.
- The suicide rates of Native American Lands are far above all the other types, with rates more than double that of some of the other types.
- Hispanic Centers and African American South communities have lower rates of suicide than the national average, even though many are rural.
What’s driving the increase in suicides among the young is not fully understood. One commonly cited factor is the rise of smartphones and social media sites and applications. Recent revelations about the toxic impacts of Facebook and Instagram, which is owned by Facebook, have made headlines. A former Facebook employee recently told Congress the company’s internal research found that 13.5% of teen girls said Instagram worsens suicidal thoughts, while 17% of teen girls said Instagram contributes to their eating disorders.
It’s too easy to blame social media entirely for these increases, however. Young people face a range of stressors in their daily lives, and the unsettled political and socioeconomic conditions in the United States in recent years may play a role.
More important, the data show that the community types with the highest youth suicide rates also seem to be the ones with higher rates of suicide for the general population. That is, the numbers suggest there is a place-driven component to the nation’s suicide epidemic linked to a variety of ground-level factors, including access to local mental health-care providers, general community attitudes toward mental health, and differing levels of family and community social capital.
Those place-based differences shed new light on this topic. While there can be little doubt that social media and the “virtual world” play roles in increasing suicide rates among the young (perhaps even a large role), the data in this report present an argument for the importance and power of the physical world. In short, the numbers suggest that where people live and the people with whom they interact in their communities matter a lot.
The ACP has written this piece in advance of our short documentary on teen suicide in rural Park County, Montana, a Graying America community near Bozeman. We sought to understand youth suicide in a rural community at the ground level by talking to people who have been impacted and witnessing how the community is addressing the problem. Early next year, the ACP plans to release the film, funded by the Blank Foundation and the Robert Wood Johnson Foundation. A short trailer is below.
The documentary and this report focus on 10- to 24-year-olds because the suicide increase in this age cohort is especially alarming. It’s a sign that the nation’s challenges around mental health and well-being — including Deaths of Despair from alcohol, drug overdose, and suicide — don’t just affect the nation’s aging white population. The challenges concern all races and ethnicities and even strike at the nation’s youngest populations.
This report is by no means the final word on the issue of youth suicide and geography, but should be an opening for further inquiry.
The Overall Numbers and the Spikes
The chart below shows the suicide rates per 100,000 people in the 10-to-24-year age group in all the ACP types since 2000, broken into five-year intervals. The bars show how the suicide rates in all 15 types have increased since 2000. Some types have experienced greater increases than others, but no community type has been immune.
Some spikes stand out, particularly the Evangelical Hubs, LDS Enclaves, and Native American Lands.
The Urban/Rural Divide
One noticeable trend in the data: suicide rates are highest among the ACP’s more rural communities. From 2015-2019, the seven community types with the highest rates of youth suicide were:
- Native American Lands (41.8 per 100,000),
- LDS Enclaves (17.3),
- Military Posts (14.4),
- Evangelical Hubs (13.9),
- Graying America (13.7),
- Working Class Country (13.4), and
- Aging Farmlands, where the rate is 22.0, but it excludes ages 10 to 14 because those data are not available due to small sample sizes.
On the other end of the spectrum, the community types with the lowest suicide rates are the most urban, the Urban Suburbs (7.9) and Big Cities (8.3).
The urban/rural differences are notable. Even excluding the Native American Lands, which are an outlier in the data (we have devoted a section to them below), the rates in the LDS Enclaves were more than twice what they were in the Big Cities and Urban Suburbs. Other rural community types are more than 60% above those urban areas.
In a sense, the higher numbers in rural America may be surprising. Rural communities are often considered tightly-knit, with strong social capital, while urban communities are described as big and impersonal. And rural communities, such as the Evangelical Hubs, LDS Enclaves, and Aging Farmlands, are places where people tend to know each other well.
However, rural places are also less likely to have easy access to mental health care. The Robert Wood Johnson Foundation’s County Health Rankings and Roadmaps shows the challenges in some communities.
- The median Big City county has one mental health-care provider for every 320 people.
- The median Evangelical Hub county has one for every 1,280 people.
- The median Working Class Country county has one for every 1,300 people.
- And there are so few mental health-care providers in the Aging Farmlands, the County Health Rankings doesn’t even measure a median.
To be clear, having more mental health-care providers in a community does not necessarily mean suicide rates are lower.
A couple of community types, the African American South and Hispanic Centers, have even fewer mental health-care providers per capita (one for every 1,310 and one for every 1,530 respectively). Both were below the national average for suicides among the young. Meanwhile, Graying America has a more mental health-care professionals per capita than other rural places, one for every 620 people, but their youth suicide rates consistently still well above the national average.
The lower numbers in the African American South and Hispanic Centers is a trend we saw in Deaths of Despair overall, as well. It may be that deeper familial or community bonds in these places help insulate them from some of the problems rural white communities face.
Why do rural communities see higher suicide rates? There are several theories.
One is isolation. Young people tend to seek out socialization and that can be harder in rural communities. Getting together with friends can be difficult when they live miles away. A related factor can be pressure to conform. On the ACP’s recent trip to Montana, people cited the pressure to fit into standard roles. For young people who are outside what’s considered the social mainstream, particularly in their sexual and gender identities, that pressure can be immense. In small schools and communities, it can be hard for those who are different to find like-minded souls.
Smartphones might actually play favorable and unfavorable roles. Young people in rural communities can use the mobile devices to connect to a much broader world, but that bigger world can also feel very distant to them.
And rural communities, often home to hunters, tend to have more guns. Firearms are the leading means of suicide in the United States.
What’s Happening in Native American Lands
The Native American Lands deserve special attention. The figures in those communities are so far above the rest of the ACP types that they don’t seem to be measuring the same data.
Overall, the figures for the Native American Lands are stark. Among 10- to 24-year-olds, more than 41 people per 100,000 took their own lives annually from 2015 to 2019. In urban areas, such as the Big Cities and Urban Suburbs, the figures look radically different for the same time period. But the figures in the Native American Lands even dwarfed numbers where the suicide among the young is bigger issue, such as LDS Enclaves, the next highest community type with a rate of 17.3 per 100,000.
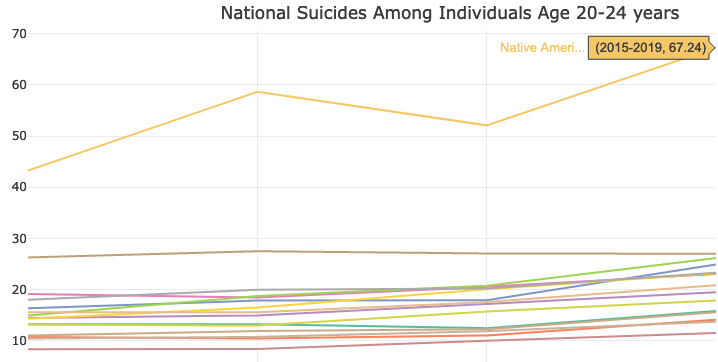
And even those numbers understate the challenges in the Native American Lands. The figures among older members of the age group, those ages 20 to 24, are extremely troubling. More than 67 per 100,000 people in that age group committed suicide annually in the Native American Lands from 2015 to 2019. The next highest community type for that age group in that period was the Aging Farmlands, where the figure was 27 per 100,000.
When you see the figures for the age group on a line chart with all the other ACP types, you get a sense of the difference.
These kinds of numbers in the Native American Lands are all too familiar in the ACP’s analyses. In our Deaths of Despair work, these communities consistently sit far above the other 14 community types. The numbers serve as a reminder of the special challenges the Native American Lands face.
Many are struggling economically due to a combination of extremely rural locales with little outside investment, low median household incomes, and low college education rates. For young people, the future can look daunting. Add into the mix a lack of mental health-care providers and the issues pile up. Veteran journalist Ray Suarez examined the complex interlocking issues in the Native American Lands in Montana earlier this year.
The numbers show that the mental health challenges begin at a young age in these communities, and would seem to argue for more money and attention on early intervention. The challenges only grow as the population ages.
Communities of Color and Other Points in the Data
One consistent point in the ACP’s work on Deaths of Despair: how a few community types stand against the broader geographic trends in the data, the African American South and Hispanic Centers. Both types tend to be rural, have lower incomes, and lower college education rates. However, their Deaths of Despair figures are consistently lower than other rural communities. That trend continues with suicides among the young.
In 2015-2019, Hispanic Centers’ 8.8 suicides per 100,000 people among 10- to 24-year-olds was close to the lower numbers in the Big Cities and Urban Suburbs. The numbers in the African American South were higher at 9.2 per 100,000, but still below the national figure (10.03) and lower than the numbers in rural white communities. And, as noted above, there are relatively few mental health-care providers in these communities. In fact, the numbers are lower in these communities than in any other, except the Aging Farmlands.
The County Health Rankings shows both of these community types score fairly high for “social associations” (that’s the number of membership associations per 10,000 population). But other community types score higher, including the Aging Farmlands, where the suicide rates are higher.
Looking at several other measures (above-average childhood poverty, below-average high school completion) young people in the African American South and Hispanic Centers face steeper challenges than those living elsewhere. Yet the lower suicide numbers suggest the data are not catching everything. There seems to be a resilience built into these communities that is worthy of more study.
Two youth-oriented communities, College Towns and Military Posts, also present interesting points to study. The ACP tends to view those communities as different sides of the same coin. Both are full of younger people at a critical juncture of their lives, usually living away from home for the first time but on very different paths.
They look quite different in the suicide data for 10- to 24-year-olds. College Towns, at 9.1 suicides per 100,000 people, were below the national average in the 2015-2019 time period, while the Military Posts at 14.5 were well above it. Much is sometimes made of the stresses young people face in college — and the 9.1 figure is higher than the numbers for the Big Cities and Urban Suburbs — but compared to other community types, the College Towns' number is actually fairly low. The number for the Military Posts, however, places it just behind the LDS Enclaves as the community type with the third-highest rate.
That higher rate in the Military Posts could be tied to a variety of other factors. For instance, some soldiers face PTSD upon returning home from the battlefield. And, of course, these communities tend to have a large number of firearms, including stores selling firearms. Guns are far and away the leading means of suicide in the country. In 2019, firearms were used in just over half of all suicides, according to data from the Suicide Prevention Resource Center. The next highest means was suffocation at 29%. It stands to reason that suicides would be higher in a community where firearms are readily available.
Also of note in the urban/rural split, there are differences within urban areas. The Big Cities and Urban Suburbs were both below the national average for youth suicides in the 2015-2019 period, but the Middle Suburbs (10.7 per 100,000) and Exurbs (11.1) were above the national average for suicides among the young. Those higher numbers are somewhat surprising, particularly in the Exurbs, where families tend to have higher incomes and more comfortable lifestyles.
One possible factor is both have fewer mental health providers than their more urban counterparts, one for every 510 people in the Middle Suburbs and one for every 840 in the Exurbs. But another factor could be that those community types have higher percentages of white, non-Hispanic people, 80% in the median Exurban county and 85% in the median Middle Suburb. As mentioned above, suicide seems to be a bigger scourge in white, non-Hispanic communities.
And, in the Exurbs in particular, there may be other pressures. On a trip to Douglas County, Colorado, an Exurb outside of Denver, we heard from local residents about the pressure to “keep up with the Joneses” and try to “have it all.” We heard those stories concerning parents, but they could well be impacting younger people as well.
Conclusions and Next
Taken together, the numbers here show the size of America’s youth suicide problem and the complexities lying under it. The differences in the ACP community types are deep. Some are densely populated and some are very rural. Some are racially and ethnically diverse and others are not. Some are wealthy and others struggle with poverty. But all saw suicides among youth rise in the past two decades.
Yet the differences between the numbers in these places are a sign that easy solutions will likely not be easy to find. Rural communities in particular seem to be facing deeper challenges, but those with large communities of color have avoided the worst numbers. Access to mental health-care providers seems to be an issue, but, looking at the data, it doesn’t appear to be determinative.
It may be that the best way to understand the differences between these places is doing much deeper research and reporting on the ground. The coming ACP short documentary on Park County, Montana, will offer an example of what that kind of look can provide and explore how one community has tried to address the problem. But there is much work to be done. The numbers laid out in this report should mark a first step toward a greater understanding of a troubling and growing problem.
